

All Tennesseans deserve affordable health care, including you. At UnitedHealthcare Community Plan, we help people live healthier lives.
We offer many plans to help Tennessee residents get healthy — and stay healthy. We cover adults, people with disabilities, expecting moms and children in Tennessee with our TennCare Medicaid plans.
Whatever plan you choose, UnitedHealthcare will help you get the care you need.
Watch the video at right to learn more about UnitedHealthcare Community Plan of Tennessee.
1 Benefits, features, and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply. Other hearing exam providers are available in the UnitedHealthcare network. The plan only covers hearing aids from a UnitedHealthcare Hearing network provider.
It’s your health. It’s your choice.
Everyone deserves affordable health care, including you.
Working adults, people with disabilities, pregnant women, and children who qualify for Medicaid should check out UnitedHealthcare Community Plan.
We have the Medicaid benefits and extras that can make a real difference in your life. All at no cost to you.
Sometimes, you might need a little extra help. Get extras not covered by Medicaid.
We also offer resources to help you make the most of your plan. Including:
Visit tn dot gov slash tenncare for more information.
Helping you live a healthier life.
We are here for you, Tennessee
Remember to choose UnitedHealthcare Community Plan.
And get the Plan that gets you more.
To learn more about UnitedHealthcare Community Plan, visit UHCCommunityPlan.com forward slash TN.



You can get the Self Care app from AbleTo at no cost. Self Care offers you:

Our TennCare Medicaid plan offers a range of benefits. Children, pregnant women, adults and people who are elderly or have a disability may qualify based on income. View the benefits below to see all that our TN TennCare Medicaid plan offers.
This plan is available wherever you live in Tennessee.
Get things like:

Tennessee CoverKids provides free, comprehensive health coverage for qualifying children age 18 and younger and pregnant women. It covers preventive health services, doctors visits, hospital visits, vaccinations, well-child visits, developmental screenings, mental health and pregnant women get prenatal, delivery, postpartum care. Children also get vision and dental care.

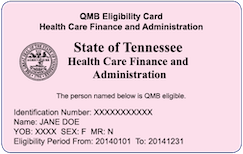
Tennesseans on a UnitedHealthcare Dual Special Needs Plan (or dual health plan) get many extra benefits beyond those you get with either Original Medicare or Tennessee Medicaid.

Behavioral health is as important as physical health. That's why we have the same coverage for both.
Required care is 100% covered with no copay. This includes:

Get the support you need to stay healthy — or to get better if you are injured or sick. Pregnant moms also get extra support to keep you and your baby healthy. Member benefits include:

Nothing is more important than the health and well-being of you and your baby. That’s why our TennCare Medicaid plan benefits include:

Make sure sight, teeth and hearing are the best they can be. Benefits include:
Vision: Covered with limits, not covered for pregnant women age 19 and older
For children under age 19, vision services are limited to:
For pregnant women age 19 and older, vision services are limited to:
Dental: For children under age 19 only, not covered for pregnant women age 19 and older
Hearing: Annual hearing screening, hearing aids are limited to 1 per ear per calendar year up to age 5, then 1 per ear every 2 years thereafter

TennCare CHOICES in Long-Term Services and Supports (or CHOICES for short) is for adults age 21 and older with a physical disability and seniors age 65 and older.
CHOICES offers services to help a person live in their own home or in the community. These services are called Home and Community Based Services or HCBS. These services can be provided in the home, on the job or in the community. They help with daily living activities and allow people to work and be actively involved in their local community. CHOICES also provides care in a nursing home if needed.
If you think you need long-term services and supports, call us at 1-800-690-1606. We may use a short screening that will be done over the phone to help decide if you may qualify for CHOICES. If the screening shows that you don’t appear to qualify for CHOICES, you’ll get a letter that says how you can finish applying for CHOICES.
Employment and Community First CHOICES (ECF CHOICES) is for people of any age who have an intellectual or developmental disabilities to live and thrive in their own community.
ECF CHOICES offers services to help people live and thrive in their own community as independently as possible. These HCBS can help with activities of daily living, employment supports and independence skills training. ECF CHOICES also offers services to help people with complex medical or behavioral support needs and families who are caring for their loved one.
If you think you need long-term services and supports and would like to apply for the ECF CHOICES Program, you can refer yourself or your loved one by here

The newsletter is a great way to learn about our health plan and important health topics. Now you can read it whenever, wherever you want. Check back quarterly for a new edition.
Medicaid Newsletter - Summer 2024
CHIP Newsletter - Summer 2024
TN Medicaid (TennCare) is health insurance for people with low incomes. You might be able to get Medicaid in Tennessee if you’re pregnant, have children or live with a disability. In some cases, other adults also may qualify. Costs to you are low and based on your ability to pay. It’s important to know that Medicaid rules and coverage differ from state to state.
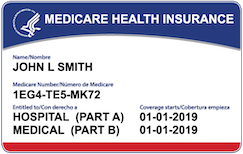
Dual Special Needs Plans (also called dual health plans or D-SNPs for short) are for people who get both Medicaid and Medicare. Dual plans cover doctor visits, hospital stays and prescription drugs. They offer more benefits and extras than Original Medicare. You’ll keep all your TennCare Tennessee Medicaid benefits, too.
Disclaimer information (scroll within this box to view)Looking for the federal government’s Medicaid website? Look here at Medicaid.gov.
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract and a contract with the State Medicaid Program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is available to anyone who has both Medical Assistance from the State and Medicare. Benefits, features and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply. Benefits, premiums and/or co-payments/co-insurance may change on January 1 of each year.
Dual Special Needs plans have a $0 premium for members with Extra Help (Low Income Subsidy).
Benefits, features, and/or devices vary by plan/area. Limitations, exclusions and/or network restrictions may apply.
This service should not be used for emergency or urgent care needs. In an emergency, call 911 or go to the nearest emergency room. The information provided through this service is for informational purposes only. The nurses cannot diagnose problems or recommend treatment and are not a substitute for your provider's care. Your health information is kept confidential in accordance with the law. The service is not an insurance program and may be discontinued at any time. Nurse Hotline not for use in emergencies, for informational purposes only.
UnitedHealthcare Connected® for MyCare Ohio (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and Ohio Medicaid to provide benefits of both programs to enrollees.
UnitedHealthcare Connected® (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and Texas Medicaid to provide benefits of both programs to enrollees.
UnitedHealthcare Connected® for One Care (Medicare-Medicaid plan) is a health plan that contracts with both Medicare and MassHealth (Medicaid) to provide benefits of both programs to enrollees.
This is not a complete list. The benefit information is a brief summary, not a complete description of benefits. For more information contact the plan or read the member handbook. Limitations, copays and restrictions may apply. For more information, call UnitedHealthcare Connected® Member Services or read the UnitedHealthcare Connected® member handbook.
UnitedHealthcare Senior Care Options (SCO) is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare and does not have any other comprehensive health Insurance, except Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our Senior Care Options (SCO) program.
Every year, Medicare evaluates plans based on a 5-Star rating system. The 5-Star rating applies to plan year 2024.
The choice is yours
We will provide you with information to help you make informed choices, such as physicians' and health care professionals' credentials. This information, however, is not an endorsement of a particular physician or health care professional's suitability for your needs.
The providers available through this application may not necessarily reflect the full extent of UnitedHealthcare's network of contracted providers. There may be providers or certain specialties that are not included in this application that are part of our network. If you don't find the provider you are searching for, you may contact the provider directly to verify participation status with UnitedHealthcare's network, or contact Customer Care at the toll-free number shown on your UnitedHealthcare ID card. We also recommend that, prior to seeing any physician, including any specialists, you call the physician's office to verify their participation status and availability.
Some network providers may have been added or removed from our network after this directory was updated. We do not guarantee that each provider is still accepting new members.
Out-of-network/non-contracted providers are under no obligation to treat UnitedHealthcare plan members, except in emergency situations. Please call our customer service number or see your Evidence of Coverage for more information, including the cost- sharing that applies to out-of-network services.
In accordance with the requirements of the federal Americans with Disabilities Act of 1990 and Section 504 of the Rehabilitation Act of 1973 ("ADA"), UnitedHealthcare Insurance Company provides full and equal access to covered services and does not discriminate against qualified individuals with disabilities on the basis of disability in its services, programs, or activities.
Network providers help you and your covered family members get the care needed. Access to specialists may be coordinated by your primary care physician.
Paper copies of the network provider directory are available at no cost to members by calling the customer service number on the back of your ID card. Non-members may download and print search results from the online directory.
To report incorrect information, email provider_directory_invalid_issues@uhc.com. This email box is for members to report potential inaccuracies for demographic (address, phone, etc.) information in the online or paper directories. Reporting issues via this mail box will result in an outreach to the provider’s office to verify all directory demographic data, which can take approximately 30 days. Individuals can also report potential inaccuracies via phone. UnitedHealthcare Members should call the number on the back of their ID card, and non-UnitedHealthcare members can call 1-888-638-6613 / TTY 711, or use your preferred relay service.
If you’re affected by a disaster or emergency declaration by the President or a governor, or an announcement of a public health emergency by the Secretary of Health and Human Services, there is certain additional support available to you.
If CMS hasn’t provided an end date for the disaster or emergency, plans will resume normal operation 30 days after the initial declaration.